The digital transformation of healthcare has introduced a variety of technologies designed to improve patient care, streamline workflows, and enhance communication between providers. Two of the most commonly used terms in this space are Electronic Medical Records (EMRs) and Electronic Health Records (EHRs). While they may sound similar, they serve different purposes and have distinct functionalities.
For healthcare providers, understanding the difference between EMRs and EHRs is critical when choosing the right system to optimize care delivery, improve patient outcomes, and meet regulatory requirements. Let's break down these two digital record-keeping systems, highlight their differences, and explain why making the shift from an EMR to an EHR can be a game-changer for your practice.
What is an Electronic Medical Record (EMR)?
An Electronic Medical Record (EMR) is a digital version of a patient’s chart, designed for use within a single healthcare practice or organization. It replaces traditional paper records and allows providers to document patient encounters, track medical histories, and manage treatment plans more efficiently.
Key Features of an EMR:
- Digital documentation of patient visits, diagnoses, and treatments.
- Tracks patient data over time for internal use.
- Automates reminders for preventive care, such as vaccinations and screenings.
- Enhances efficiency by reducing paperwork and improving recordkeeping.
Despite its benefits, an EMR has one major limitation—it is confined to a single practice. If a patient visits another provider, their medical history is not automatically accessible. This lack of interoperability often results in fragmented care, delays in treatment, and the need for manual transfer of records via fax or email.
What is an Electronic Health Record (EHR)?
An Electronic Health Record (EHR) is an advanced version of an EMR, designed to be interoperable—meaning it can be securely shared across multiple healthcare organizations, including specialists, hospitals, labs, and pharmacies.
Key Features of an EHR:
- Includes all the information found in an EMR but allows data sharing across different providers and locations.
- Provides a comprehensive, real-time view of a patient’s health history.
- Supports collaboration between healthcare professionals for better-coordinated care.
- Helps providers meet government regulations for value-based care models.
By enabling seamless data exchange, EHRs ensure that all authorized providers involved in a patient’s care have access to up-to-date, complete medical records. This leads to better-informed decisions, reduced duplication of tests, and improved patient outcomes.
EMR vs. EHR: What’s the Difference?
The primary difference between EMRs and EHRs lies in how patient information is shared. While EMRs store patient data within a single practice, EHRs extend access across multiple healthcare settings.
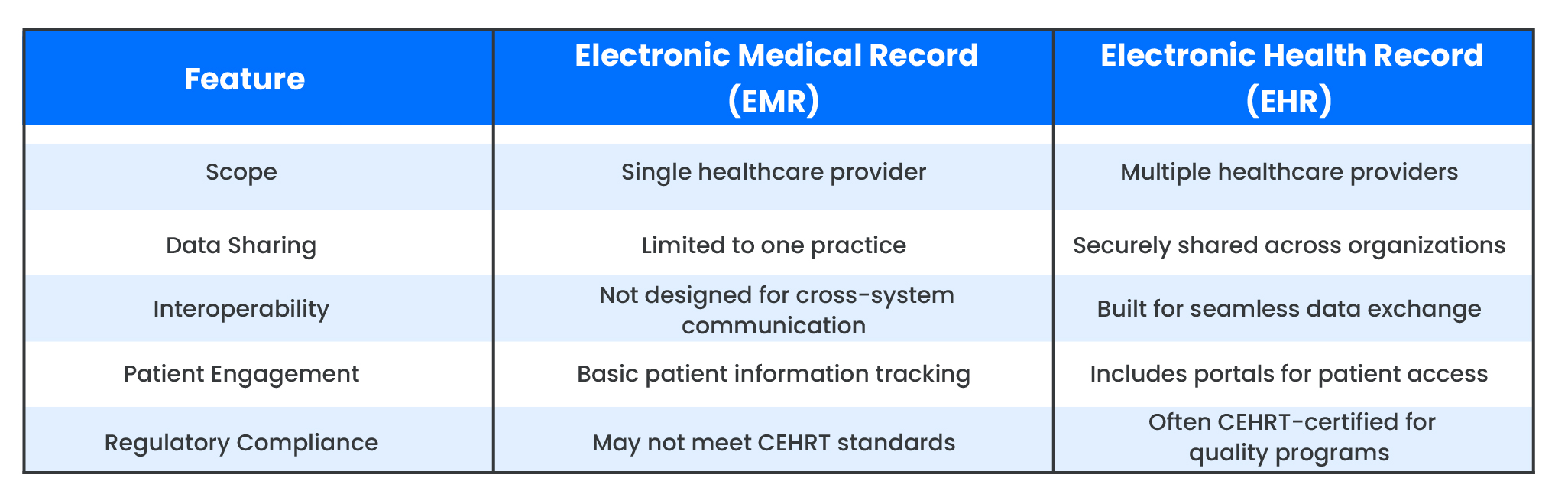
While an EHR encompasses everything an EMR does, not all EMRs are equipped to function as an EHR due to their limited data-sharing abilities. If a system does not allow for easy information exchange across providers and healthcare networks, it is considered an EMR rather than an EHR.
The Benefits of Upgrading from an EMR to an EHR
Many healthcare providers initially adopted EMRs to comply with early digital record-keeping requirements. However, as the industry shifts towards value-based care and care coordination, the need for interoperable EHR systems has become essential. Here’s why transitioning from an EMR to an EHR can benefit your practice:
1. Better Provider Visibility into Patient Records
EHRs enable multiple providers to access up-to-date patient data in real time, helping improve decision-making and reduce duplication of efforts.
2. Better Patient Outcomes
Access to a patient's full medical history enables more accurate diagnoses, timely treatments, and better health monitoring. By reducing the chances of miscommunication or missing information, EHRs contribute to safer, more effective care.
3. Increased Efficiency & Reduced Administrative Burden
EHRs automate routine tasks such as appointment scheduling, prescription refills, and clinical documentation. Some advanced systems even integrate AI-powered transcription and voice recognition to reduce the time spent on charting.
4. Enhanced Data Security & Compliance
Certified Electronic Health Record Technology (CEHRT) ensures compliance with HIPAA regulations and industry standards for data security. EHRs use encryption and access controls to protect sensitive patient information while allowing authorized personnel to access records securely.
5. Support for Value-Based Care & Regulatory Requirements
Government healthcare programs, such as those administered by the Centers for Medicare & Medicaid Services (CMS), require EHR adoption to participate in quality initiatives. Practices using EHRs can track quality measures, submit reports more efficiently, and qualify for financial incentives.
EHR vs. Patient Portals: Are They the Same?
EHRs are often associated with patient portals, but they are not the same. A patient portal is an online tool that allows individuals to access their medical records, communicate with providers, schedule appointments, and request prescriptions.
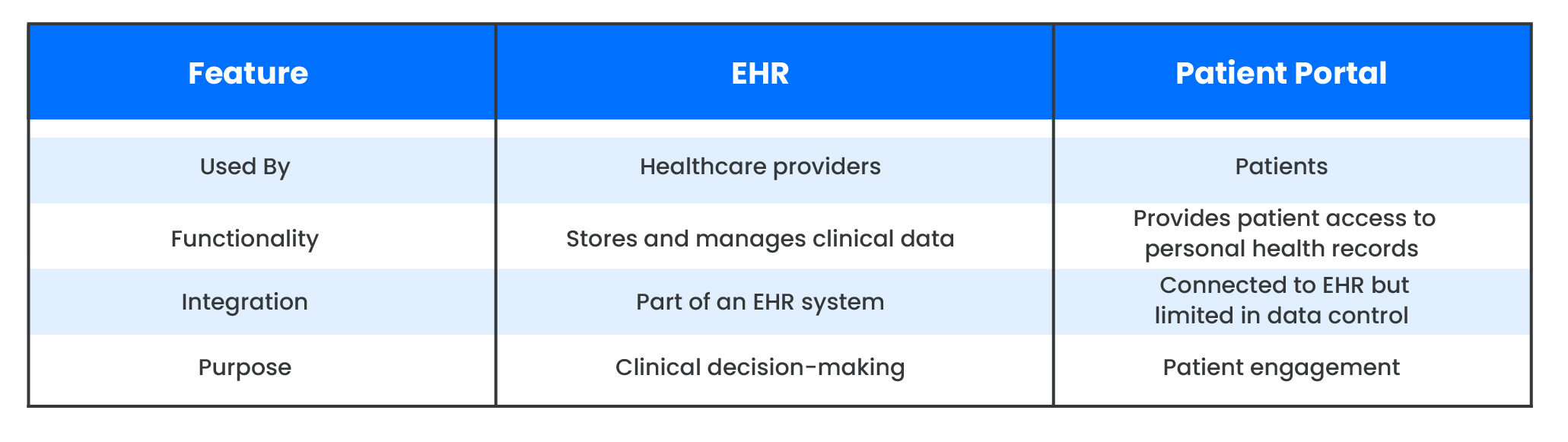
While EHRs support healthcare providers, patient portals empower patients by giving them better control over their health information. Many modern EHR systems include built-in patient portals, bridging the gap between providers and their patients.
Is It Time to Upgrade from an EMR to an EHR?
For medical practices still using EMRs, now is the time to consider the advantages of upgrading to an EHR system. With increasing demands for interoperability, efficiency, and value-based care, making the switch can streamline operations, improve patient outcomes, and ensure compliance with healthcare regulations.
If you’re exploring EHR solutions, look for a system that offers:
- Seamless integration with other healthcare systems.
- Advanced automation to reduce administrative workload.
- Certified compliance with healthcare regulations.
- Scalability to support future practice growth.
Healthcare technology is rapidly evolving, and adopting an EHR is no longer just an option—it’s a necessity for staying ahead in an increasingly connected medical landscape.
Final Thoughts
The distinction between EMRs and EHRs goes beyond just terminology; it reflects a fundamental shift in how healthcare providers manage patient data. While EMRs serve as digital versions of paper charts, EHRs take it a step further by enabling comprehensive, coordinated care across multiple providers.
For healthcare practices looking to enhance efficiency, compliance, and patient care, investing in a robust EHR system is a smart move. Whether you're upgrading from an EMR or implementing an EHR for the first time, choosing the right system can transform the way you deliver healthcare—for both providers and patients alike.